- alnoormedia1992@gmail.com
- 01324254572
Glaucoma
Advancing Glaucoma Treatment with State-of-the-Art Technology
Glaucoma, a chronic eye condition affecting millions worldwide, requires specialized care and advanced treatment approaches. At Al-Noor Eye Hospital, we understand the significance of providing comprehensive glaucoma services that incorporate the latest technology. Our hospital is committed to utilizing state-of-the-art advancements to ensure accurate diagnosis, effective management, and optimal outcomes for our patients.
At Al-Noor Eye Hospital, we prioritize accurate and early diagnosis of glaucoma, as timely intervention can prevent irreversible vision loss. We employ advanced diagnostic technology, such as optical coherence tomography (OCT) and visual field testing, to assess the extent of optic nerve damage and monitor disease progression. These non-invasive tests allow our highly skilled ophthalmologists to precisely evaluate your condition, enabling personalized treatment plans that address your specific needs.
When surgical intervention becomes necessary, Al-Noor Eye Hospital harnesses the power of innovative technology to deliver exceptional results.
Beyond diagnosis and treatment, Al-Noor Eye Hospital provides comprehensive care and ongoing management for glaucoma patients. Our multidisciplinary team collaborates to ensure that you receive holistic care, addressing not only the physical aspects but also the emotional and psychological impact of the condition. We emphasize regular follow-up visits and individualized treatment plans to monitor disease progression, adjust therapies, and optimize outcomes over time.
Patient-Centric Approach:
At Al-Noor Eye Hospital, our patient-centric approach is at the heart of everything we do. We understand the challenges and concerns associated with glaucoma, and we are committed to supporting you throughout your treatment journey. Our compassionate and knowledgeable staff will guide you, ensuring that you have a clear understanding of your condition, treatment options, and ongoing management strategies. We are here to answer your questions, address your concerns, and empower you to take an active role in your eye health.
Glaucoma in Details
Overview:
Glaucoma is a group of conditions characterized by a progressive loss of vision. Glaucoma is classified as primary or secondary. The most common type of glaucoma, called “primary” open angle glaucoma, is a chronic disturbance of the normal fluid pressure inside the eye and is generally age-related. “Acute” or secondary closed angle glaucoma is rarer and is identified by a sudden, painful shutting down of the mechanisms controlling intraocular fluid pressure. In “secondary” glaucoma, factors such as trauma, certain drugs, infections, tumors or advanced cataracts cause an increase in the intraocular fluid pressure.
Glaucoma is the second leading cause of blindness worldwide. It is a heterogeneous group of disorders marked by damage to the structural or functional integrity of the optic nerve that causes characteristic atrophic changes. Over time, this may also lead to specific visual field defects. Damage can be arrested or diminished by adequate lowering of intraocular pressure (IOP). Yet, some debate still exists as to whether IOP should be included in the definition of glaucoma, as some subsets of patients can exhibit the characteristic optic nerve damage and visual field defects while having an IOP within the normal range. PRESSURES DO NOT DETERMINE IF YOU HAVE GLAUCOMA. You can have normal or low pressure and have glaucoma. It is thought up to 50% of people with glaucoma have normal tension glaucoma. Your eye doctor must examine your optic nerve head to diagnose glaucoma.
Classification:
- PRIMARY OPEN-ANGLE GLAUCOMA
Primary open-angle glaucoma (POAG) is a major worldwide health problem. It is usually non-symptomatic and progressive in nature, and is one of the leading preventable causes of blindness in the world. With early screening and treatment, POAG can usually be diagnosed and its progress stopped before significant vision loss occurs.
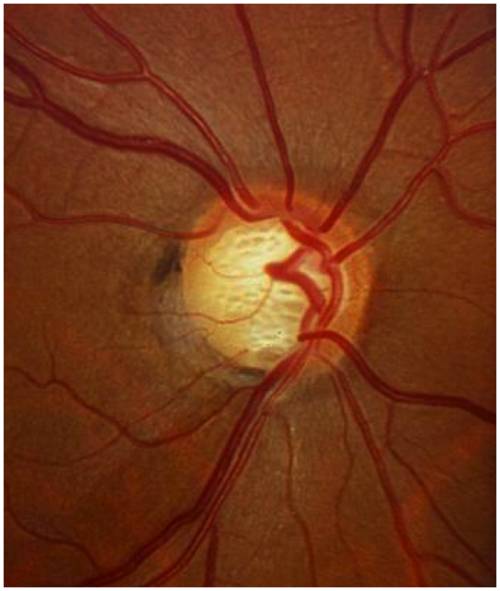
POAG is distinctly a multifactorial optic neuropathy that is chronic and progressive with a characteristic loss of optic nerve fibers and cupping and atrophy of the optic disc. The loss of optic nerve fibers is associated with open anterior chamber angles, visual field abnormalities, and IOP that is too high for the continued health of the eye.
Elevated IOP is a risk factor associated with the development of POAG but it is not the disease itself. As with other forms of glaucomatous neuropathies, the exact cause of POAG is not known. Many risk factors have been identified, including elevated IOP, family history, race, age older than 40 years, and myopia. Elevated IOP is the most studied because it is the most clinically treatable risk factor for glaucoma.
- ANGLE-CLOSURE GLAUCOMA
Angle-closure glaucoma (ACG) is a condition in which the iris is opposed to the trabecular meshwork at the angle of the anterior chamber of the eye. Angle-closure relates to anatomic factors in the anterior segment (shallow anterior chamber, crowded drainage angle, pupil block) compounded by pathophysiologic events. The iris may be pushed forward into contact with the trabecular meshwork, as in pupillary block or plateau iris, or it may be pulled anteriorly, as occurs with other inflammatory conditions. The position of the iris in either case causes the normally open chamber angle to close. Aqueous humor that should drain out of the anterior chamber is trapped inside the eye. Pain, blurred vision, and nausea may occur if the ensuing rise in pressure is sudden.
Damage occurs potentially both to outflow pathways and to the optic nerve head. This causes a dramatic and painful rise in IOP. If closure of the angle occurs suddenly, symptoms are severe and dramatic. Acute ACG is an emergency and immediate treatment is essential to prevent damage to the optic nerve and loss of vision. If closure occurs intermittently or gradually, ACG may be confused with chronic open-angle glaucoma. Intermittent episodes of ACG over a long period of time will cause glaucomatous damage to the optic nerve.
- Pseudoexfoliation Glaucoma
Deposits of a fibrillary material that may contribute to the obstruction of the fluid drainage from the eye.
- Pigmentary Glaucoma
Pigment dislodged from the iris obstructs the eye’s drainage structures.
- Angle Recession Glaucoma
Scar tissue from previous trauma obstructs the outflow of fluid.
- Neovascular Glaucoma
Various disorders cause blood vessels to proliferate on the iris and in the eye’s drainage structures.
- Normal Tension Glaucoma
Glaucoma that develops despite eye pressure in the normal range.
- Childhood Glaucoma or Pediatric Glaucoma
Childhood glaucoma, also referred to as congenital glaucoma, pediatric glaucoma or primary infantile glaucoma occurs in babies and young children.
Symptoms of Glaucoma:
In most cases, glaucoma is asymptomatic (has no symptoms). By the time an individual experiences decreased vision, the disease is frequently in its latter stages. Since early warning signs of glaucoma are rare, it is important —- especially for those at risk —- to have regular medical eye examinations every one or two years.
Patients with chronic glaucoma may not be aware of any symptoms because the disease develops slowly and they rarely notice loss of peripheral vision. Patients with an acute form of glaucoma (acute angle closure) may develop severe symptoms because ocular pressure rises quickly and they may experience:
- Blurred vision, especially at night
- Halos or rainbows around lights
- Severe headaches or eye pain
- Nausea
Glaucoma Risk Factors:
Although glaucoma is most common in adults over the age of 40, susceptibility is not determined by age alone. A genetic predisposition of those with a family history of the disease and African-Americans, are at a particularly increased risk. Studies have shown individuals at greater risk for glaucoma may fit one or more of the following criteria:
- Are over the age of 60
- Have a family history of the disease, elevated intraocular pressure
- Are African-American over the age of 40
- Have diabetes or hypertension
- Are very nearsighted or farsighted
- Steroid Users
- Have had an eye injury
- Are Asian
- Are Hispanic over the age of 60
Diagnosis:
To achieve an accurate assessment, experienced ophthalmologists perform a comprehensive glaucoma screening that consists of non-invasive, pain-free procedures:
- Tonometry
This test measures the pressure inside your eye.
- Visual Field
The visual field test determines whether you have difficulty seeing in any areas of your peripheral vision — the areas on the side of your visual field. There are a few different types of visual field tests:
- Confrontation visual field exam.
Your eye doctor sits directly in front of you and asks you to cover one eye. You look directly at your eye doctor while he or she moves his or her hand in and out of your visual field. You tell your doctor when you can see his or her hand or fingers.
- Tangent screen exam.
You sit a short distance from a screen and stare at a target at its center. You tell your doctor when you can see an object move into your peripheral vision.
- Automated perimetry.
Your eye doctor uses a computer program that flashes small lights as you look into a special instrument. You press a button when you see the lights.
- Spectral Domain OCT
Newer diagnostic studies using computer-imaging technology such as spectral domain optical coherence tomography (OCT), now permit precise measurements of the retinal nerve fiber layer that cannot be visualized by the unaided human eye. This test helps monitor and detect optic nerve loss over time.
- Optic Disc Photography
Optic nerve photographs document the severity of damage to the nerve and are used to monitor changes over time.
- Pachymetry
Because corneal thickness can influence your eye pressure reading, this test measures the thickness of your cornea.
- Gonioscopy
This exam looks at the drainage angle in your eye.
Treatment:
- Pharmacologic Treatment (1st Option)
Medications for the treatment of glaucoma are aimed at lowering IOP through two mechanisms, decreasing AH production and increasing AH outflow. It is recommended that IOP be lowered to a target level. That level is generally 20% below the baseline as measured several times. Prostaglandin analogues and beta-blockers are currently the most frequently used agents. Due to their once-daily dosing and effectiveness, prostaglandin analogues are generally selected as first-line options in treatment.
- Beta-blockers. Topical beta-blockers are one of the most commonly used classes of medications in the treatment of POAG. They produce an IOP-lowering effect by reducing the production of AH by the ciliary body.
- Prostaglandin Analogues. Topical prostaglandin analogues are usually the first choice by prescribers for POAG. In a large meta-analysis, it was concluded that prostaglandin analogues showed a greater 24-hour IOP reduction than timolol and other POAG medications.
- Adrenergic Agonists. Dipivefrin is a nonspecific adrenergic agonist. It is a prodrug of epinephrine and decreases IOP by increasing AH outflow through the uveoscleral route and trabecular meshwork. Dipivefrin is less effective at lowering IOP than other treatment options and is poorly tolerated. Therefore, it is rarely used.
- Cholinergics. Cholinergic agents lower IOP by increasing AH outflow through the trabecular meshwork. These agents are rarely used because of multiple daily dosing and adverse effects. The local adverse events include retinal detachment, myopia, miosis, and pupillary block. Systemic side effects would be typical cholinergic effects such as sweating, salivation, nausea, vomiting, diarrhea, and bradycardia.
- Carbonic Anhydrase Inhibitors. These agents lower IOP by blocking the secretion of sodium and bicarbonate ions into the AH, thereby inhibiting the production of AH. Topical formulations (brinzolamide and dorzolamide) are considered for monotherapy or adjunctive therapy in those who do not achieve effective control with other medications. These are well tolerated, with adverse events including transient burning and stinging, blurred vision, tearing, and corneal edema.
- Cholinesterase Inhibitor. The cholinesterase inhibitor echothiophate widens the trabecular meshwork by inhibiting the destruction of acetylcholine and lowers IOP by increasing AH outflow. Side effects are a major reason for limited use. These include fibrinous iritis, iris cysts, conjunctival thickening, and nasolacrimal occlusion. In addition, this drug has limited commercial availability and should only be used in nonresponsive patients.
- Combination Products. Products that combine timolol with brimonidine or dorzolamide are available. A product that combines brimonidine and brinzolamide is also available. Combination therapy should be considered when initial therapy produces only a partial response. Advantages of using one product instead of two include less total preservative exposure, no washout effect, a single copay, and a possible improvement in adherence to treatment.
- Preservative-free Products. Recent research has shown that preservatives like benzalkonium chloride (BAK) in eyedrops could be causing a significant increase in local adverse events, such as dry eyes. These studies also showed that preservative-free eyedrops lead to a significant decrease in local adverse events.
- Nonpharmacologic Treatment (2nd Option)
- Laser Trabeculoplasty. This procedure is considered in patients who fail to be adherent to medication regimens, are unable to administer eyedrops, or cannot tolerate topical medications. Trabeculoplasty uses a very focused beam of light to cause increased drainage through the trabecular meshwork. The effects of this may wear off over time and, therefore, long-term benefit is uncertain.
- Trabeculectomy. This is the most common surgical procedure used to lower IOP. It involves creating a new pathway for the drainage of AH via bypassing the trabecular meshwork. Trabeculectomy is generally considered after topical agents and trabeculoplasty have been deemed insufficient at controlling IOP. It may also be considered as an initial therapy when IOP is extremely elevated.
- Cyclodestructive Procedures. These are used when medicaland surgical treatments have failed and glaucoma is highly advanced. During cyclodestructive procedures, the ciliary body is intentionally damaged so that AH production is permanently reduced.




1/9 E Block Lalmatia, Dhaka- 1207 Tel:(02)58153763
© 2023 Al Noor Eye Hospital, All Rights Reserved
